The eating disorders of anorexia nervosa and bulimia nervosa are characterized by severe disturbances in body image, eating, and engaging in compensatory behaviors that result in serious medical, psychological, and social problems. For example, eating disorders increase the risk of obesity, nutritional deficiencies, depression and anxiety disorders, chronic pain, osteoporosis, insomnia, neurological symptoms, cardiovascular problems, substance abuse, and death. The criteria for anorexia nervosa include an intense and unrealistic fear of becoming fat, engaging in behaviors intended to produce distinct weight loss, and amenorrhea resulting from the refusal to maintain a healthy weight. The body-image disturbance and consequential denial of the negative health effects of one’s low weight are defined as maintaining a weight that is less than 85% of what is considered an ideal body weight for the individual’s age, gender, and height. This denial is evident by a physiological criterion of amenorrhea that is defined as the absence of at least three consecutive menstrual cycles for women.
Two specific types of anorexia nervosa, restricting type and binge-eating–purging type, are based on how the extreme low weight is reached and maintained. The restricting type is defined as the absence of bingeing and purging behaviors. The binge-eating–purging type states that during the current episode of anorexia nervosa, the individual also engages in binges (eating inappropriately massive amounts of food in one set period of time) or purging behavior (self-induced vomiting, misuse of laxatives, diuretics, or enemas). While anorexia nervosa can affect men and women of any age, race, and socioeconomic and cultural background, the occurrence of anorexia nervosa is 10 times higher in the female population than among males.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
The criteria for bulimia nervosa are similar to that of anorexia in that they also outline an intense fear of becoming fat, but they differ by including the requirements of powerful urges to overeat and subsequent binges that are followed by engaging in some sort of compensatory behavior in an attempt to avoid the weight gain effects of excessive caloric intake. The fear experienced by an individual with bulimia nervosa is also in regard to body-image disturbance. The paradox is the presence of the uncontrollable urges to overeat, resulting in binges. These binges are defined as occurring within 2 hours and eating an amount of food that is larger than most people would consume in a similar time and setting coupled with a sense of lack of control (inability to stop eating) during the binge. Both the body-image disturbance and binges result in engaging in compensatory behaviors to evade weight gain. Compensatory behaviors are separated into purging and nonpurging types. Purging behaviors include self-induced vomiting, use of laxatives, diuretics, enemas, or medication abuse. In comparison, nonpurging behaviors include fasting or excessive exercising. A qualification for a diagnosis of bulimia nervosa is that the binge eating and inappropriate compensatory behaviors must occur, an average, at least twice a week for 3 months. In contrast to those with anorexia nervosa, people with bulimia nervosa are able to maintain body weight at or above a minimal normal level.
Bulimia nervosa is considered to be less life threatening than anorexia nervosa; however, the incidence of bulimia nervosa is higher. Bulimia nervosa is nine times more likely to occur in women than men. The vast majority of those with bulimia nervosa are at normal weight. Antidepressants are widely used in the treatment of bulimia nervosa. Patients who have bulimia nervosa are often linked with having impulsive behaviors involving overspending and sexual activity, as well as having family histories of alcohol and substance abuse and mood and eating disorders.
Eating disorders exist and develop on a continuum with health detriment occurring throughout the entire span of the development and maintenance of the disorder. That is, cognitions and behaviors seen in full-blown disorders begin with less frequency or intensity and subsequently increase as the disorder develops. While the antecedents and causes of eating disorders are myriad and complex, excessive exercise has been the focus of much research and clinical attention. Although study design and quality have varied greatly, researchers typically find that a large percentage of individuals with eating disorders engage in excessive exercise. Thus, this entry will primarily focus on the relationship between excessive exercise behavior (exercise dependence) and eating disorders. Note that the entry on the female athlete triad focuses on eating disorders and athletes.
Of importance, according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR), exercise becomes excessive when “it significantly interferes with important activities, when it occurs at inappropriate times or in inappropriate settings, or when the individual continues to exercise despite injury or other medical complications” (American Psychiatric Association, 2000, pp. 590–591). This definition, however, fails to quantify the amount needed to determine if exercise is excessive. Because excessive exercise and its negative health outcomes have been studied far less than the other diagnostic symptoms, more research is needed to better understand excessive exercise and eating disorders. In an attempt to provide clarity to the excessive exercise construct, researchers advocate for either revising the diagnostic criteria with regard to excessive exercise, or eliminating excessive exercise as a diagnostic criterion because of lack of empirical support for it. In short, considerable debate exists regarding eating disorder classification in general, and in particular with excessive exercise, regarding how best to define it, or even whether to include excessive exercise as a compensatory behavior for bulimia nervosa.
Relationship Between Excessive Exercise and Eating Disorders
Current exercise guidelines identify the minimum amount of exercise needed to experience health benefits. The guidelines also recommend that an increased amount of exercise is associated with additional benefits. Although increases above the minimum guidelines are encouraged, no consensus exists on how much is too much, that is, at what point any further increase in exercise may have a negative effect on one’s health.
By definition, a regimen of exercise that has become detrimental to an individual’s physical and psychological health constitutes excessive exercise or exercise dependence. Simply stated, exercise dependence is a craving for leisure-time physical activity, resulting in uncontrollably excessive exercise behavior that manifests itself in physiological (e.g., tolerance) or psychological (e.g., withdrawal) symptoms. Characteristics of exercise dependence include exercising despite either injury or illness; experiencing withdrawal effects when an exercise session is missed; and giving up social, occupational, and family obligations to exercise. Exercise dependence may also play a pivotal role in explaining the function of exercise behavior in the development and maintenance of eating disorders.
The relationship between exercise and eating pathology, however, is complex and controversial. Diagnostic criteria, correlational research, and clinical observation show a higher prevalence of exercise in individuals with bulimia nervosa and anorexia nervosa than in non-eating-disordered samples. This is in part because of exercise’s ability to offset caloric intake, resulting in weight loss. For many individuals beginning to experience an eating disorder, diet and compensatory behaviors, such as picky eating, skipping meals, and fasting, may only reduce the number of calories consumed. Consequently, weight loss is slowed and the individual may seek complementary methods to accelerate weight loss. If progress with weight loss seems slow, compulsive exercise may be added in an attempt to increase weight loss. While this seems reasonable and sufficient to explain the role of exercise in eating disorders, simply examining the amount of exercise does not explain either why or to whom excessive exercise may become problematic. Thus, more recent investigations reveal that psychological factors such as exercise dependence may better explain the role of exercise in eating disorders. Therefore, a closer examination of prevalence rates and psychological factors indicates a much more complicated relationship between exercise and eating disorders.
The belief that exercise is associated with the development and maintenance of eating disorders is based largely on cross-sectional, retrospective, and case study designs that fail to adequately assess and quantify excessive exercise. For example, there is a long standing clinical observation that most hospitalized inpatients receiving treatment for anorexia nervosa engage in excessive amounts of exercise during the development or maintenance of their eating disorder. However, no definition is provided for what is considered excessive exercise. Similarly, recent studies have correlated participation in athletics (populations that engage in large amounts of physical activity) with deleterious eating attitudes related to eating disorders. Thus, researchers have focused on exercise amount contributing to the development and maintenance of eating disorders. However, focusing on exercise amount may be misleading because much of the research examining excessive exercise has relied on biased sampling methods using unvalidated self-report exercise measures that lack a clear, concise, and consistent definition of how much exercise is excessive. Furthermore, many of the operational definitions used for excessive exercise fail to meet the minimum amount of exercise needed to achieve the health-related benefits of physical activity.
Primary Versus Secondary Dependence and Eating Disorders
Most of the research examining the relationship between excessive exercise and eating disorders has focused on the amount of exercise contributing to the development of eating disorders but has overlooked psychological variables that may mediate such a relationship. Understanding the psychological antecedents of exercise may help clarify the relationship between eating disorders and excessive exercise by offering insight into the distinction between primary versus secondary exercise dependence. Primary exercise dependence occurs when the individual meets criteria for exercise dependence and continually exercises solely for the psychological gratification resulting from the exercise behavior. Secondary exercise dependence occurs when an exercise dependent individual uses increased amounts of exercise to accomplish some other end, such as weight management or body composition manipulation.
Simply stated, it is important to distinguish whether the individual is exercising excessively to satisfy the need to exercise (primary dependence) or if they are engaging in increased amounts of exercise as a compensatory behavior that is secondary to other pathology, such as an eating disorder (secondary dependence). Because exercise can be used as a compensatory behavior to prevent or reverse weight gain, secondary exercise dependence in the context of eating disorders occurs when individuals meet the criteria for exercise dependence and continually exercises to manipulate and control their own body; thus, exercise dependence is secondary to an eating disorder. Recently, researchers have found that exercise dependence symptoms, not exercise behavior, mediate the relationship between exercise and eating pathology. Thus, psychological factors, not the amount of exercise, may better explain why the exercise dependence–eating disorder relationship exists.
The Exercise and Eating Disorders Model
The limitations of biased clinical observations, retrospective research designs, vague operational definitions of excessive exercise, inconclusive animal research, and overlooking potential mediating psychological variables support the need for theoretically driven models that explain the relationship between eating disorders and the psychological motivation as well as the physical effects of exercise.
Previous models have been advanced that postulate how and why obligatory attitudes toward exercise may influence the development and maintenance of eating pathology and disorders. However, these models offer limited insight into why the benefits typically experienced as a result of regular exercise do not occur in eating disorders. For example, exercise may impart positive improvements on the eating disorder risk factors of anxiety, body image, depression, stress reactivity, and self-esteem in non-eating-disordered populations. Similarly, cardiovascular benefits, such as increased cardiac mass, increased stroke volume and cardiac output at rest and during exercise, lower resting heart rate and blood pressure, and a decreased tendency for blood clotting are pertinent to eating disorder research because cardiac damage can occur early during eating disorder development. Exercise also has the ability to reduce adiposity, thus contributing to a leaner, more fit, and culturally ideal body type. Moreover, sociocultural pressures to be thin and social comparison are risk factors for the development of eating disorders. Furthermore, the metabolic benefits of exercise include decreased triglycerides and increased high-density cholesterol, increased insulin mediated glucose uptake, and a possible increase in resting metabolism. Finally, exercise increases skeletal muscle mass and bone density in youth and it is related to the retention of bone mineral density in older adults. This has implications in the development of osteoporosis, a common consequence of prolonged eating disorder behaviors. Thus, exercise is an effective intervention for many physical and psychological health issues, and yet recent recommendations for research to reexamine the role of exercise in eating disorders have been largely overlooked.
Heather Hausenblas, Brian Cook, and Nickles Chittester presented a conceptual model examining such aforementioned relationships (see Figure 1). Their Exercise and Eating Disorders Model states that regular exercise is associated with improvements in several physical (cardiovascular, metabolic benefits, decreased adiposity, and increases in bone density), psychological (body image, depression, anxiety, stress reactivity, and self-esteem), and social benefits that are also risk factors, maintenance factors, outcomes, or diagnostic criteria for eating disorders. Hence, this exercise and eating disorders model has consolidated and supported several narrative and meta-analytic reviews that have shown exercise’s ability to impart positive improvements on eating disorder risk, development, and maintenance factors. The model also extends our current understanding of the relationship of exercise and health status by including exercise dependence. That is, exercise dependence may explain why the development of eating disorders may supersede the expected benefits of exercise. Simply stated, this model posits that in the absence of pathological psychological factors such as exercise dependence, the benefits conveyed by regular exercise—improvements in depression, anxiety, stress reactivity, self-esteem, and body composition—may counteract the risk factors for eating disorders like body dissatisfaction, depression, anxiety, and increased body mass.
Recent research by Cook and colleagues, Hausenblas, Daniel Tuccitto, and Peter Giacobbi, has provided initial support for this exercise and eating disorder model, revealing that the psychological health benefits, conveyed by exercise can reduce the risk of eating disorders.
First, university students completed self-report measures of physical and psychological quality of life, exercise behavior, eating disorder risk, and exercise dependence symptoms. Structural equation modeling analysis found support for the mediation effect of exercise dependence on eating disorders as well as the effect of psychological well-being on eating disorders. Together, exercise behavior, psychological well-being, and exercise dependence symptoms predicted 22.9% of the variation in eating disorders. Thus, these results indicated that the psychological health benefits conveyed by exercise reduced eating disorders. These results were replicated in a more diverse sample of college students in another study by Cook and various colleagues in 2011.
Exercise Interventions and Eating Disorders
The initial tests of the Exercise and Eating Disorders Model suggest that the model may synthesize two divergent lines of research. That is, exercise may play a role in the development of eating disorders when exercise dependence is simultaneously present. Similarly, the psychological health benefits of exercise may also reduce eating disorder risk for individuals without exercise dependence.
Conclusion
Preliminary research has found that mild to moderate exercise appears to attenuate eating disorder symptoms in patients suffering with anorexia or bulimia nervosa. However, before exercise interventions are considered mainstream, future randomized controlled trials are needed to establish a dose–response relationship for exercise and identify the conditions (e.g., type or severity of eating disorder, minimum weight level, and exercise environment) under which an exercise intervention may be undertaken. Interest in exercise dependence and eating disorders is recent but provides a context as to why the relationship between exercise and other pathologies, such as body-image disturbance and eating disorders, exists.
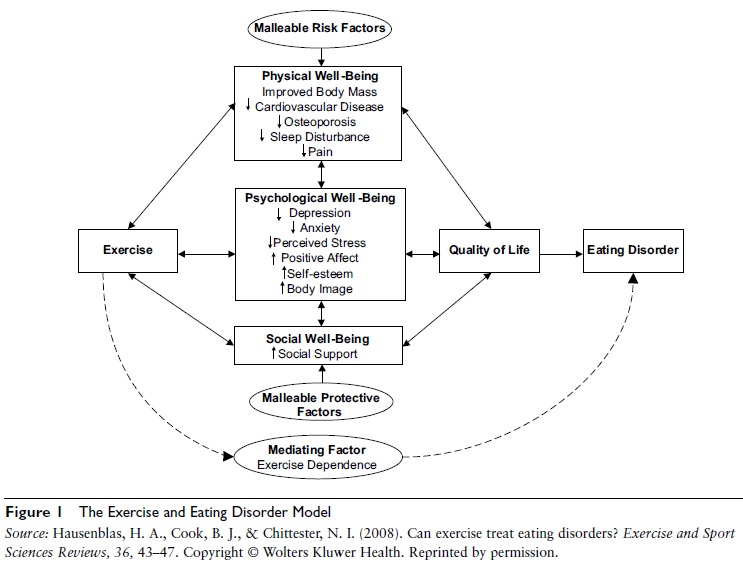
Figure 1 The Exercise and Eating Disorder Model
References:
- Adkins, C. E., & Keel, P. K. (2005). Does “excessive” or “compulsive” best describe exercise as a symptom of bulimia nervosa? International Journal of Eating Disorders, 38, 24–29.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text revision). Washington, DC: Author.
- Cook, B. J., & Hausenblas, H. A. (2008). The role of exercise dependence for the relationship between exercise behavior and eating pathology: Mediator or moderator? Journal of Health Psychology, 13, 495–502.
- Cook, B. J., & Hausenblas, H. A. (2011). Eating disorder specific health-related quality of life and exercise in college females. Quality of Life Research, 20(9), 1385–1390. doi: 10.1007/s11136-011-9879-6
- Cook, B. J., Hausenblas, H. A., Tuccitto, D., & Giacobbi, P. (2011). Eating disorders and exercise: A structural equation modeling analysis of a conceptual model. European Eating Disorders Review, 19, 216–225.
- Dalle Grave, R., Calugi, S., & Marchesini, G. (2008). Compulsive exercise to control shape or weight in eating disorders: Prevalence, associated features, and treatment outcome. Comprehensive Psychiatry, 49, 346–352.
- Hausenblas, H. A., & Fallon, E. A. (2006). Exercise and body image: A meta-analysis. Psychology and Health, 21, 33–47.
- Hausenblas, H. A., Cook, B. J., & Chittester, N. I. (2008). Can exercise treat eating disorders? Exercise and Sport Sciences Reviews, 36, 43–47.
- Hausenblas, H. A., & Symons Downs, D. (2002). Exercise dependence: A systematic review. Psychology of Sport and Exercise, 3, 89–123.
- Holm-Denoma, J. M., Scaringi, V., Gordon, K. H., Van Orden, K. A., & Joiner, T. E. (2009). Eating disorder symptoms among undergraduate varsity athletes, club athletes, independent exercisers, and nonexercisers. International Journal of Eating Disorders, 42, 47–53.
- Meyer, C., Taranis, L., & Touyz, S. (2008). Excessive exercise in the eating disorders: A need for less activity from patients and more from researchers. European Eating Disorders Review, 16, 81–83.
See also: