Birth weight is the actual weight of the baby determined immediately after delivery. The average birth weight in the United States varies between 3,000 and 3,600 g, depending on factors such as race, size of the parents, and gender (boys are heavier). Birth weight distribution of 150,000 deliveries between the years 1988 and 2002 in southern Israel is shown in Figure 1, with a mean of 3,200 g. Estimated fetal weight can be calculated in utero by ultrasound, based on fetal weight percentile, according to previously established gestational age. Fetal weight increases especially during the second half of pregnancy.
Estimated fetal weight less than the 10th percentile is considered small for gestational age, which may be due to intrauterine growth restriction. Low birth weight, defined as less than 2,500 g, has contributed appreciably to neonatal morbidity including neurological and intellectual deficits. However, such morbidity exists specifically in extremely low birth weight newborns (<1,000 g). It is estimated that 3 to 10% of infants are growth restricted. An important determinant of fetal weight is inheritance, and indeed a small woman is likely to have a small baby. Socioeconomic status of the mother is an important determinant of birth weight. Socioeconomic deprivation is associated with lower fetal growth rate, basically due to smoking, alcohol, or other substance abuse and poor nutrition. Other possible causes for growth restriction are problems in the placenta (which carries food and blood to the baby), birth defects and genetic disorders, maternal infections, hypertensive disorders, and even several toxins and medications.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
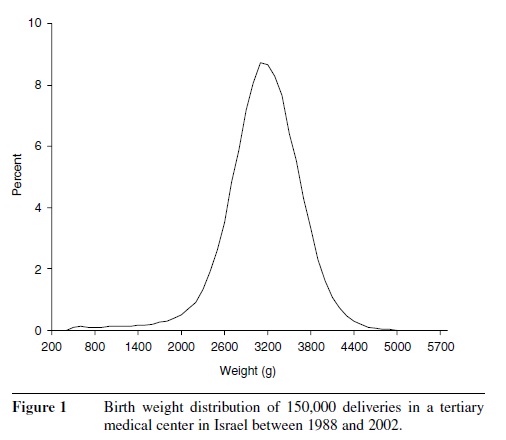 Figure 1 Birth weight distribution of 150,000 deliveries in a tertiary medical center in Israel between 1988 and 2002.
Figure 1 Birth weight distribution of 150,000 deliveries in a tertiary medical center in Israel between 1988 and 2002.
Management of growth restriction includes an attempt to determine the underlying etiology, including a careful ultrasound search for malformations. Fetal karyotype should be considered if structural anomalies are present. Also, testing for infectious diseases such as rubella, varicella, CMV, syphilis, HIV, and toxoplasmosis should be performed. Obvious environmental toxins or drugs should be removed from the maternal environment. Women are encouraged to cease smoking, eat a variety of healthy foods, and achieve optimal weight gain during pregnancy, as determined by their prepregnancy weight for height. Fetal surveillance includes serial ultrasound scans and fetal heart rate monitoring. Unfortunately, interventions to improve blood flow to the uterus (including bed rest and low-dose aspirin) failed to improve fetal outcome in randomized studies.
The fetus with enhanced growth is defined by birth weight greater than the 90th percentile for gestational age. Macrosomia is a term used to describe a very large baby and is defined as birth weight of more than 4,000 g. Macrosomia can be ascribed to an exaggerated, linear fetal growth or to abnormal maternal glucose homeostasis (diabetes mellitus). This high birth weight may cause birth trauma due to a serious condition known as shoulder dystocia—difficulty delivering the infant’s shoulder. Although complicating only 0.13 to 2.1% of all deliveries, shoulder dystocia is associated with adverse maternal and fetal outcomes. Maternal morbidity includes lacerations of the birth canal and postpartum bleeding. Fetal complications include fracture of the clavicle or humerus and neurological complications such as asphyxiation or Erb’s palsy. Several clinicians investigated factors associated with shoulder dystocia in an attempt to predict its occurrence. Major risk factors documented by most studies include fetal macrosomia, maternal diabetes, obesity, and operative delivery. Diabetic patients are almost five times more likely to have a shoulder dystocia, mainly due to higher rates of fetal macrosomia, larger shoulder and extremity circumferences, and increased body fat.
Unfortunately, prediction and therefore prevention of shoulder dystocia is virtually impossible. There is no reliable way to detect macrosomia in uteri since ultrasound has a wide deviation of up to 22% in fetal macrosomia. Thus, an accurate estimate of excessive fetal size is not possible, and the diagnosis
is generally made after delivery. Reduction in the time interval from delivery of the head to the delivery of the body of the baby is important for survival. Several maneuvers exist to deliver the anterior shoulder and relieve shoulder dystocia, which are familiar to the attending obstetrician. Most cases are handled successfully.
References:
- American Academy of Family Physicians, http://www.aafp.org
- American College of Obstetricians and Gynecologists, http://www.acog.org
- Gilbert, W. , & Danielsen, B. Pregnancy outcomes associated with intrauterine growth restriction. American Journal of Obstetrics and Gynecology, 188, 1596–1601.
- Langer, , Berkus, M. D., Huff, R. W., & Samueloff, A. (1991) Shoulder dystocia: should the fetus weighing greater than or equal to 4000 grams be delivered by cesarean section? American Journal of Obstetrics and Gynecology, 165, 831–837.
- Sheiner, , Levy, A., Katz, M., Hershkovitz, R., Leron, E., & Mazor, M. (2004). Gender does matter in perinatal medicine. Fetal Diagnosis and Therapy, 19, 366–369.