There are several prevailing models that connect psychological factors and sport injury, each with slightly different perspective on relevant biological, psychological, or social factors. Moreover, prevailing models have typically focused either on incorporating psychosocial factors in predicting and preventing sport injury incidence or upon identifying psychosocial factors associated with injury recovery and rehabilitation outcomes. Extensive reviews of these models have been written by Jean Williams and Mark Andersen, Britton Brewer, and Diane Wiese-Bjornstal. This entry provides an overview of the mediating biological pathways and physiological mechanisms linking psychosocial stress to athletic injury and, where appropriate, other adverse health consequences.
Both historical and recent conceptualizations of psychosocial stress posit wide-ranging biological effects on health. In this regard, Frank Perna and colleagues have argued that emotional, behavioral, and physiological aspects of stress response must be considered together with attention disruption to fully capture potential pathways mediating the relationship between psychosocial stress and adverse health including athletic injury. Additionally, since the physical demands of training volume and intense exercise required in competitive athletics are known to have adverse temporal effects on immune, neuroendocrine, and skeletal muscle repair response, a primary tenet of a biopsychosocial model of injury is that psychosocial distress may act synergistically with high intensity, high-volume sports training to widen a window of susceptibility to illness or injury.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
The biopsychosocial model of stress athletic injury and health (BMSAIH) is offered below to illustrate pathways between stress demands and athlete health (see Figure 1). The BMSAIH expands the Andersen and Williams model of psychosocial stress and athletic injury in three essential ways: (1) It clarifies mediating physiological pathways between athletes’ stress response and adverse health outcomes (e.g., sport injury); (2) it considers other health outcomes and behavioral factors that impact sport participation as well as injury; and (3) it integrates the impact of exercise training upon athletes’ health.
The BMSAIH should be considered an independent extension of Andersen and Williams’s classic model of stress and athletic injury, which is reviewed elsewhere (see also the entry “Injury, Psychological Susceptibility to”). Similar to other generic models of stress and adverse health consequences, the Andersen and Williams model posited that a stress response mediated the effect of stressor(s) on the health outcome, athletic injury, with the stress response being composed of physiological and cognitive features (attentional perturbations such as peripheral narrowing) thought to predispose an athlete to injury. While the stress response was conceptualized as being both physiological and cognitive in nature, the original model and the preponderance of studies have principally only researched cognitive features (disturbances in attention and recognition of sport-related cues) thought to predispose an athlete to injury. Yet, the relationship between psychosocial stress and athletic injury appears stronger for overuse injuries that are likely less dependent on cognitive processing and more likely related to physiological processes affecting exercise training adaptation and recovery. The stress-injury model also proposed a number of factors, such as personality, history of stress, and coping resources, that may moderate a stress response, but there was less clarity and exposition of mediating pathways, particularly those related to stress physiology, by which stress response may increase risk of injury.
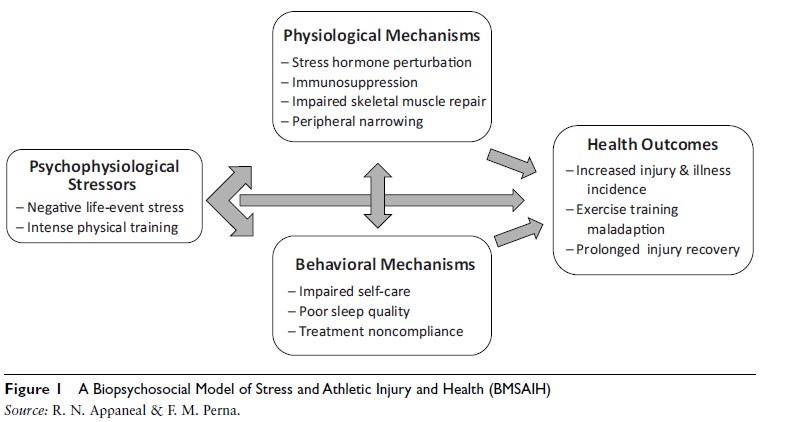
Figure 1 A Biopsychosocial Model of Stress and Athletic Injury and Health (BMSAIH)
Source: R. N. Appaneal & F. M. Perna.
Stress Response Mechanisms
Negative life stress and attendant emotional distress, through autonomic nervous system (ANS) response pathways, is thought to exacerbate the adverse effects of prolonged high-intensity and high-volume exercise. Specifically, psychological stress causes activation of the ANS yielding the release of catecholamines like epinephrine, norepinephrine, neuropeptides, and glucocorticoids (cortisol). Because target organs, such as heart, vasculature, muscle, and immune tissue, contain efferent nerves and have receptors for catecholamine and glucocorticoids, ANS activation affects target organs either by direct innervation of the parasympathetic and sympathetic nervous systems (PNS and SNS, respectively) or by hormonal action via activation of the hypothalamic-pituitary-adrenal-cortex (HPAC) and cortisol release. Cognitive features related to a person’s appraisal of the severity of a stressor and the capacity to cope with a stressor is known to exacerbate or prolong emotional reactivity and concomitant physiological response. Direct innervation, particularly by the SNS and catecholamine release, and hormonal action (e.g., cortisol release) thus provide the mechanistic links used to explain how the brain and associated cognitive– affective processes attendant to psychological stress may influence stress physiology and other physical systems, particularly those of relevance to athlete health like immune and skeletal muscle.
Because the ANS may operate either through direct innervation or hormonal action, there are a variety of possible neuroendocrine and hormonal patterns (differential responses to stress) that have evolved to characterize the stress response since Hans Selye first proposed the general adaptation syndrome, an undifferentiated response to stress. Moreover, specific ANS patterns are known to be influenced by features of cognitive appraisal particularly being dependent if an individual views a life event as a negative stressor or as a challenge. Thus, it is recognized that ANS activation in response to stress is not always deleterious, and indeed, is necessary. For example, it has long been known that ANS activation, particularly of the SNS, is associated with performance of physical and cognitive tasks. Similarly, HPAC activity and cortisol release are known to potentiate the actions of epinephrine in the completion of physical tasks and, when not prolonged, cortisol initiates a cascade leading to anabolic activity necessary for muscle repair following intense exercise.
A thorough discussion of possible hormonal response patterns in response to stress is beyond the scope of this entry but can be found in work by Trent Petrie and Frank Perna. In short, three hormonal patterns are thought to result in adverse health effects. These are thought to occur when individuals (a) experience frequent negative life stress and concomitant frequent activation of the SNS and HPAC pathways involving principally the release of epinephrine and cortisol to a lesser extent, (b) are hypersensitive to stressors and have an atypically high SNS and epinephrine response out of proportion to the magnitude of a stressor, and (c) experience chronic stressors and emotional distress with a prolonged activation of the HPAC and heightened cortisol release. The latter scenario involving measurement of enduring effects of negative life events, either in isolation or with their association with cortisol response, has received the most attention.
In addition to stress mechanisms described above, HPAC activation and possible concomitant behavioral disruptions (e.g., sleep disturbance) resulting from heightened negative affect may act in synergy with the demands of heavy exercise to increase risk of illness and injury. For example, poor sleep has been associated with prolonged elevation in evening cortisol, immune decrements, and lessened growth hormone release, all of which may inhibit muscle repair following acute exercise. Negative emotion-linked increases in stress hormones (cortisol) and behavioral perturbation may thus widen or prolong a window of susceptibility for illness and injury that is created by high-intensity and high-volume training. That is, psychological distress may impair muscle growth and repair processes by prolonging the presence of post-exercise catabolic hormones like cortisol that also impair immunity and inhibit the secretion and action of anabolic factors, such as growth hormone and insulin-like growth factors. Due to cortisol’s immunosuppressive and muscle catabolic effects, prolonged training-induced cortisol elevation may create favorable conditions for viral infection, athletic injury, and exercise training maladaptation.
Similarly, elevated negative mood state, particularly fatigue and depression, has been used to identify overtrained athletes. Depressed mood has also been related to impaired immune function, and this effect may be mediated by cortisol elevation. Although the physiological strain of exercise training is largely responsible for cortisol and mood fluctuation, studies suggest that psychological life-event stress (LES) may also modulate cortisol and health parameters in athletes. For example, elite athletes with high LES, in comparison to low LES athletes, have been reported to experience prolonged post-exercise cortisol elevation, which was prospectively correlated with a greater frequency of physical symptom, such as muscle pain, back tightness, or flu-like symptoms. Elevated LES has also been prospectively related to increased risk of athletic injury and viral infection (e.g., common cold). In essence, the BMSAIH suggests that health effects of psychosocial stress would be most pronounced when an athlete was either in or just removed from a high-volume or high-intensity period of training, and that sport training cycle should be considered to optimally measure the association between psychosocial stress and athletic injury and adverse health.
Taken together, the literature indicates that independent from intensity and volume of sports training, psychological stress likely contributes to athletes’ neuroendocrine and immune activity, which may be a mediating pathway linking stress to increased risk for adverse health effects including athletic injury. However, the effects of psychosocial stress on health may be more pronounced during periods of high-volume and intense exercise training. Because athletes must train at high volumes and intensities to make the physiological adaptations necessary for competitive success, commercially available exercise recovery monitoring systems have appeared on the competitive sports milieu and have been extensively reviewed by Michael Kellman. These systems include the assessment of physical, emotional, and social– contextual stress responses, as athletes must maintain a delicate balance between demands and recovery to stay healthy, avoid injury, and ultimately perform optimally. However, athletes’ efforts to balance training and recovery occur within a sport culture that often undervalues the importance of psychosocial factors, and perhaps also recovery. As a result, the culture of competitive sport reinforces an imbalance between psychosocial and sport training factors, which ultimately may affect training adaptation, injury, and overall health. Sport psychology personnel trained to assist athletes with life-event, precompetitive, and post-injury stress are also widely available. However, the efficacy of psychosocial intervention to reduce injury risk, facilitate exercise-training adaptation, and enhance athlete health has been less extensively investigated.
Psychological Interventions
In the athletic domain, cognitive–behavioral stress management (CBSM) intervention in the form of psychological skills training is well known to reduce competitive anxiety and enhance athletic performance. CBSM has also been shown to reduce pain and speed recovery and return to play following arthroscopic surgery among injured recreational athletes. In a handful of randomized controlled trials, CBSM improved exercise training adaptation in the form of lessened fatigue, depressed mood, and cortisol curve during a high-volume training period among competitive rowers. Further, CBSM intervention has also been shown to reduce actual incidence of athletic injury and illness. One of these trials conducted by Perna and colleagues specifically tested if intervention effects on cortisol and affect mediated health outcomes. Findings demonstrated that rowers in a CBSM condition had significantly fewer days injured or ill and half the number of health and training center visits compared with controls. Mediation analyses indicated that modulation of affect and cortisol accounted for approximately one half and one fifth, respectively, of the intervention effect on days injured or ill. Though limited, the extant literature provides compelling support for the potential value of intervention to lessen risk of athletic injury and illness and to facilitate sports-training adaptation. Future research should seek to further elucidate the physiological pathways underpinning the psychosocial stress and health relationship, and explore biopsychosocial mechanisms that may be responsible for intervention effects on athlete health.
References:
- Brewer, B. W. (2010). The role of psychological factors in sport injury rehabilitation outcomes. International Review of Sport and Exercise Psychology, 3(1), 40–61.
- Clow, A., & Hucklebridge, F. (2001). The impact of psychological stress on immune function in the athletic population. Exercise Immunology Review, 7, 5–17.
- Kellmann, M. (2010). Preventing overtraining in athletes in high-intensity sports and stress/recovery monitoring. Scandinavian Journal of Medicine & Science in Sports, 20(Suppl. 2), 95–102.
- Perna, F. M., Antoni, M. H., Baum, A., Gordon, P., & Schneiderman, N. (2003). Cognitive behavioral stress management effects on injury and illness among competitive athletes: A randomized clinical trial. Annals of Behavioral Medicine, 25, 66–73.
- Perna, F. M., Antoni, M. H., Kumar, M., Cruess, D. H., & Schneiderman, N. (1998). Cognitive-behavioral intervention effects on mood and cortisol during exercise training. Annals of Behavioral Medicine, 20, 92–98.
- Perna, F. M., & McDowell, S. L. (1995). Role of psychological stress in cortisol recovery from exhaustive exercise among elite athletes. International Journal of Behavioral Medicine, 2(1),13–26.
- Perna, F. M., Schneiderman, N., & LaPerriere, A. (1997). Psychological stress, exercise, and immunity. International Journal of Sports Medicine, 18(Suppl. 1), S78–S83.
- Petrie, T. A., & Perna, F. M. (2004). Psychology of injury: Theory, research, and practice. In T. Morris & J. J. Summers (Eds.), Sport psychology: Theory, application, and issues (2nd ed., pp. 547–551). Hoboken, NJ: Wiley.
- Wiese-Bjornstal, D. M. (2010). Psychology and socioculture affect injury risk, response, and recovery in high-intensity athletes: A consensus statement. Scandinavian Journal of Medicine & Science in Sports, 20, 103–111.
- Williams, J. M., & Andersen, M. B. (2007). Psychosocial antecedents of sport injury and interventions for risk reduction. In G. Tenenbaum & R. C. Eklund (Eds.), Handbook of sport psychology (3rd ed., pp. 379–403). Hoboken, NJ: Wiley.
See also: