During the prenatal period, a human develops from a single cell to a complex array of living tissues and structures. Every experience a prenatal organism has, and every substance it encounters, can potentially alter the course of development. This period of dramatic changes sets the stage for postnatal outcomes, from birth to death. The longest period of prenatal development is referred to as the fetal period, during which time the developing organism is called a fetus.
When Does The Fetal Period Begin?
The first 2 weeks of life are called the period of the zygote. This period begins when a sperm and egg unite their genetic material in a single cell. The newly fertilized egg spends the first week of its existence traveling down the fallopian tube toward the uterus. As it travels, the original cell divides into multiple cells. The zygote spends the second week of its existence implanting into the wall of the uterus, which triggers hormonal changes in the mother to help maintain the pregnancy.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% OFF with 24START discount code
Once uterine implantation is complete, the developing organism is called an embryo. The period of the embryo lasts from week 3 to week 8. During this time, the embryo develops physical features that make it look human, such as eyes, ears, arms, and legs. Inside, the internal organs begin to form and function. The heart begins to beat within the first 3 weeks of gestation.
The final and longest stage of prenatal development is called the period of the fetus. This period begins during the ninth week, when bone cells begin to replace cartilage, and will last until birth. During this time, the fetus will increase rapidly in size, growing from little more than an inch in length to the size and appearance of a newborn infant.
What Happens During The Fetal Period?
Physical Changes
At the start of the fetal period, all of the organs have been differentiated. The task of the fetal period is to strengthen and integrate their functioning. In other words, the pieces are in place; all that is left are the final touches. One way to conceptualize these changes is to consider pregnancy as occurring in three trimesters, with each trimester lasting 3 months.
First Trimester
The first month of the fetal period is the last month of the first trimester. The fetus doubles in length during this time and begins to take on more human characteristics. The head becomes more erect, and the back straightens and becomes less curled in appearance. As the body grows bigger, the fetus’s large head looks more proportional, although it is still one third the length of the entire body. Details such as fingernails and toenails are added during the third month. The skin becomes less transparent, and facial structures move into place. Eyelids form, although the eyes will not open until later.
Connections form between muscles and brain, which allows for more coordinated movement patterns. Bone cells begin to manufacture blood cells. The digestive system begins producing insulin and digestive enzymes. The fetus is moving toward life outside of the womb.
Second Trimester
At the start of the second trimester, gender can usually be determined by ultrasound, the use of high-frequency sound waves that produce an image of the fetus. Sexual development actually begins much earlier, during the embryonic period, when the testes begin to form in male embryos and ovarian follicles form in female embryos. During the third month of gestation, the testes release testosterone, which triggers male embryos to develop a penis and scrotum. Because female fetuses have no testes to release these hormones, female fetuses develop a vagina about a week after male fetuses develop a penis.
A second important event during the second trimester is the onset of sensory functioning. In mammals, the sensory systems become functional in an invariant sequence. The sense of touch begins at about 8 to 10 weeks of gestation. Maria Fitzgerald at London University has found that fetuses have more irritable nerve fibers than do newborns, which may make them more responsive to prenatal stimulation. Taste and smell begin to function at about 14 weeks. Fetuses show facial responses to sweet or bitter chemicals injected into the amniotic fluid. Fetuses show visible responses to sound as early as 24 weeks, with a preference for high-frequency sounds that will last throughout infancy. Fetuses respond to light by 26 weeks, although the ability to focus will continue to improve following birth. The eyes of the fetus and newborn will remain blue until a few weeks of postnatal light exposure activate the eye pigmentation to create the adult eye color.
Physical details are also added during the second trimester. For example, fingerprints form by the fourth month. During the fifth and sixth months, eyebrows, eyelashes, and hair appear. During this same time period, the fetus’s skin is protected from the amniotic fluid by vernix caseosa, a thick, waxy covering. Vernix sticks to the skin because the fetus’s skin is covered by downy hair called lanugo. Lanugo will decrease in the seventh month, replaced by head hair, whereas vernix will still be visible at birth on the infant and in the amniotic fluid.
Third Trimester
The final trimester is when the fetus gains the most weight and length. The bones harden, consisting of more bone cells and less cartilage. A layer of fat grows under the skin, which will help the newborn infant stay warm in the postnatal environment. Hair, fingernails, and toenails grow. The fetus is also taking advantage of antibodies in the mother’s blood. These antibodies enter the fetal circulatory system through the umbilical cord and provide protection for newborn infants until they can develop antibodies of their own.
The typical length of gestation is 38 weeks; however, babies born before this time can survive. The point at which a fetus can survive outside of the womb is called the age of viability. With today’s technology, the age of viability can be as early as 22 weeks of gestation, although premature infants often face challenges that full-term infants do not face. For example, lungs finalize their development, becoming capable of breathing air at about 26 weeks. Infants born before the final trimester need assistance breathing. The earlier a fetus is born, the more developmental challenges it is likely to face.
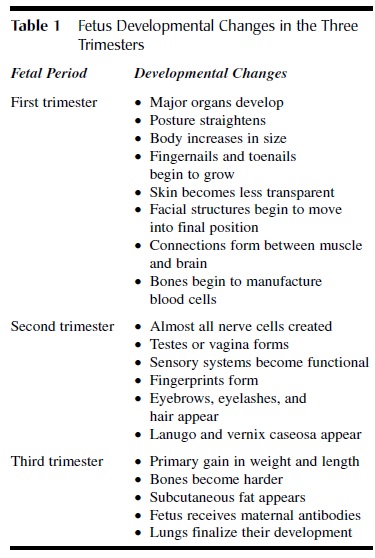 Table 1 Fetus Developmental Changes in the Three Trimesters
Table 1 Fetus Developmental Changes in the Three Trimesters
Behavioral Changes
The human fetus is an active creature. It kicks, rotates, and somersaults. The fetus also can turn its head, make faces, form a fist, suck its thumb, and curl its toes. The capability for movement begins during the second month of life; however, much of this early movement is spontaneous rather than in response to environmental stimulation. During the fetal period, movement begins to become more intentional and responsive. By the end of the second trimester, the fetus will make sucking motions in response to a touch on the lips and will shield its eyes in response to a bright light.
Some researchers have argued that behavioral patterns may tell us something about a fetus’s personality or later behavior. For example, Janet DiPietro and her colleagues demonstrated that male fetuses tend to be more active than female fetuses, which is a difference often noted in young children. Fetuses of women who report high levels of stress also exhibit higher levels of prenatal behavior. Each mother may notice a behavioral pattern that is unique to her fetus, with some fetuses being awake and active at certain times of the day and not at others.
Movement can be an important developmental tool because the ability to move increases as a consequence of movement itself. For example, as the fetus swallows and inhales amniotic fluid, it is strengthening the muscles it will use to breathe air in the postnatal world. Bones and muscles gain strength and function through their use, so that movements transition from being uncoordinated to smooth and coordinated.
Movement increases in frequency until about 17 weeks of gestation, at which time it declines. This reduction in movement may be the result of the maturation of inhibitory abilities in the brain. Movement peaks again between weeks 26 and 32, and then declines as delivery approaches. The reduction in movement that occurs late during the prenatal period is most likely due to space restrictions in the uterus. Early in development, the fetus moves freely in its amniotic sac. By the end of late prenatal period, the fetus fills the expanded uterus, and its movements can be seen through the mother’s abdominal wall. In preparation for birth, most fetuses move into an upside-down position, with their head pointed in the direction of the birth canal and their face angled toward their mothers’ spine.
Cognitive Changes
The nervous system, which includes the brain, is also rapidly developing during the fetal period. By the end of the fifth month, almost all of the brain cells that a human will have in his or her lifetime are already created. These brain cells are called neurons. Neurons that are used will develop connections with other neurons, whereas neurons that are not used will be pruned. One brain area that grows the most is the cerebral cortex, the outer surface of the brain that is more developed in humans than in other species. This growth will continue during infancy and childhood.
Important aspects of brain growth occur during sleep. We now know that fetuses not only sleep, they also dream. Dream sleep, also called rapid-eye-movement (REM) sleep, is the time when neurons form connections. These connections are even more critical to cognitive functioning than is the number of neurons an individual has. REM sleep is also a time when areas associated with learning show high levels of activity.
Research with both humans and animals has demonstrated that fetuses can learn in the womb. In a classic study by Anthony DeCasper and Melanie Spence, mothers read The Cat in the Hat out loud during the last 6 weeks of pregnancy. After birth, their infants could suck on a nipple to hear recordings of their mother reading this familiar story or an unfamiliar story. The infants who had heard The Cat in the Hat during the prenatal period sucked on the nipple in order to hear the familiar story. This behavior suggests that the infants remembered what they had heard while they were still fetuses. Prenatal learning may also explain why newborns prefer hearing their mother’s voice instead of other voices and prefer hearing their native language instead of other languages.
What Does The Mother Experience During The Fetal Period?
Although drastic changes are occurring to the fetus, the expectant mother may not feel like she is carrying another person in her body early during pregnancy. Her hormones, however, are already changing her body to maintain the pregnancy. One of the first symptoms she may experience is morning sickness, which typically occurs during the first trimester. Morning sickness may protect an expectant mother by making her more reluctant to eat foods that would be potentially harmful to the developing fetus. Women who experience morning sickness are less likely to miscarry or have a child with birth defects.
At about the 16th week of gestation, as the fetal bones begin to harden, the mother is able to feel the fetus moving. The detection of the first movement is called the quickening. First-time and heavier mothers may wait longer to feel this first movement. Early movements feel like a slight flutter or bubbling sensation. As the fetus develops, the movements get stronger, and the space in which to move gets smaller. Thus, later movements feel more recognizable, such as a small person kicking the abdominal wall.
As the fetus grows, the demands on the expectant mother increase. Her heart will get stronger and beat faster in order to supply nutrients and oxygen to the developing fetus. As the fetus grows, it will compress the organs in her chest upward, into smaller and smaller spaces, leaving the mother short of breath. During late pregnancy, the fetus drops lower in the pelvis. This change in position alleviates some of the pressure on the lungs but increases pressure on the bladder, resulting in more frequent urination.
The growth of the fetus also contributes to weight gain during pregnancy. The average woman will gain 25 to 30 pounds during a healthy pregnancy. Women who are very thin at the outset of pregnancy may gain more, whereas women who are overweight at the outset of pregnancy are often encouraged to gain less. During the final trimester, when the fetus is gaining length and weight, the mother may gain a pound per week. About two thirds of her ultimate weight gain will reflect the weight of the fetus, placenta, expanded uterus, and supporting fluids (e.g., blood and amniotic fluid).
Threats To Fetal And Maternal Health
Prenatal development is a complicated and delicate process, which can be disrupted by harmful substances ingested, inhaled, or absorbed by the mother. These substances are called teratogens. The effect that a particular teratogen will have depends on many factors, such as amount, duration, and timing of the substance. Even small amounts of substances that are tolerable to adults may be detrimental to developing organisms. The embryonic period is typically considered the most vulnerable period of development because body structures are being created during that time. The risk for developmental damage is usually lower during the fetal period, yet there are some organs and systems that are particularly susceptible.
Determining the exact results that a substance will produce is a challenging field of research. First, many risk factors occur simultaneously. For example, a woman who is taking illegal drugs may also have poor eating habits, which makes it difficult to determine which behavior resulted in a specific consequence for the fetus. A second issue for research is that genes and environment interact. For example, fetuses with a particular gene and whose mothers smoke are more likely to develop cleft palate. Third, many consequences do not appear immediately. Delayed consequences are called sleeper effects. For example, embryos and young fetuses exposed to DES (diethylstilbestrol), a drug given to prevent miscarriage, do not show symptoms until adulthood, when women are at risk for cervical cancer and both men and women are at risk for fertility problems.
Drugs
The term drug can be applied to a wide variety of substances, from prescription medication to over the counter remedies to illegal chemicals. Drugs from any of these categories have the potential to be harmful to a developing fetus.
Illegal and Prescription Drugs
Illegal drugs can alter the course of development as well as create a dependency in the developing organism. For example, prenatal exposure to cocaine is linked to premature birth, low birth weight, respiratory problems, and heart deformities. Fetuses exposed to heroin show withdrawal symptoms at birth, including vomiting, shaking, and irritability. Heroin continues to exert negative effects by slowing the rate of motor development.
A classic example of a prescription drug that proved harmful is thalidomide. Thalidomide was widely prescribed in the 1950s and 1960s as a mild sedative and antidote for morning sickness. At that time, doctors believed thalidomide to be harmless to the developing fetus. Unfortunately, thousands of exposed infants were born with limb defects, deafness, facial deformities, dwarfism, and brain damage. Many of these infants died during the prenatal period or shortly after birth. Thalidomide has recently received renewed attention, because of its ability to treat symptoms of nausea, cancer, and leprosy. Controversy exists over whether such drugs can be administered with a guarantee that they will not be made available to pregnant women.
Nicotine
Any form of tobacco (e.g., cigarettes or chewing tobacco) can have negative consequences for both the expectant mother and the fetus. Nicotine interferes with the woman’s ability to absorb certain nutrients and also causes her blood vessels to contract. When blood flow is constricted, the fetus receives less oxygen and nutrients. Nicotine has also been shown to disrupt fetal sleep patterns, particularly REM sleep. Women who smoke are more likely to have abnormalities of the placenta and to miscarry. Infants who are born of smoking mothers are more likely to have low birth weight, respiratory illness, or cleft palate. Smoking has also been linked to sudden infant death syndrome (SIDS) and attention deficit hyperactivity disorder (ADHD). Even exposure to secondhand smoke has been linked to outcomes such as asthma, bronchitis, and ear infections.
Alcohol
According to the Academy of Pediatrics, about 20% of women consume alcohol while pregnant. Some controversy exists about whether small amounts of alcohol are dangerous during pregnancy; however, research clearly demonstrates that large amounts of alcohol consumption are unsafe for the developing organism. One of alcohol’s most damaging effects is that it interferes with cell division and cell communication, both critical components of development. Alcohol also decreases the blood supply to the fetus. Because the amount that is considered harmful is not presently known, the best advice for a pregnant woman is to avoid alcohol.
Large amounts of alcohol consumption, considered to be more than 4 ounces several times a week, result in a pattern of deficits called fetal alcohol syndrome (FAS). Children with FAS tend to have slow development, mental retardation, behavioral problems, and heart problems. In addition, FAS results in a small head with an atypical facial pattern of widely spaced eyes, a thin upper lip, an upturned nose, and a flat nose bridge. Children who exhibit these characteristics to a lesser degree have fetal alcohol effects (FAEs) or alcohol-related neurodevelopmental disorders (ARNDs). These less severe effects can include low birth weight, heart and respiratory abnormalities, attention problems, learning disabilities, and behavioral disorders.
Infectious Disease
Pregnant women may be exposed to viral or bacterial infections, such as the common cold or the flu, that do not adversely affect development. However, some infections, such as syphilis, rubella, and toxoplasmosis, can directly affect the development of the fetus. Other infectious diseases, such as gonorrhea and genital herpes, target the fetus as it passes through the birth canal into the postnatal world. Acquired immune deficiency syndrome (AIDS) is a disease that can affect the fetus in the womb and the infant passing through the birth canal.
Syphilis is a fatal disease for the developing organism. About 50% of fetuses of infected mothers die during the prenatal period or shortly after birth. Survivors are at risk for problems with their central nervous system and damage to their teeth and bones.
Rubella, or German measles, has differential effects depending on the time of exposure. Rubella is most damaging during the first trimester, when it can cause a range of defects including blindness, deafness, mental retardation, and heart defects. During the second trimester, rubella is associated with hearing and vision loss as well as language difficulties. Today, most children receive a vaccination for rubella, which means most pregnant women have been protected against the disease.
Toxoplasmosis also has differential effects depending on the timing of exposure. Pregnant women may contract this parasitic infection through eating undercooked meat or from touching the feces of infected cats. During the first trimester, toxoplasmosis causes death or severe eye or brain damage, whereas later exposure leads to less severe damage of the same areas. Pregnant women are advised to make sure that the meat they eat is thoroughly cooked and to avoid contact with any area where cats defecate (i.e., litter or soil).
AIDS is a viral disease that is transmitted to some fetuses, but not to others. The factors that determine which fetuses will contract it are not completely understood. Fetuses that do contract it quickly show symptoms. As young infants, they are prone to respiratory illnesses, fever, weight loss, delayed development, and motor disturbances. Most infants with AIDS die within the first year of life. The only drug currently available (AZT) that reduces the chances of prenatal infection also can cause birth defects.
The infectious diseases discussed thus far have noticeable effects on both the mother and the fetus; however, minor bacterial infections have been identified as one of the leading causes of premature labor. For example, women with gum disease have six times as high risk for premature birth as women without gum disease. Bacterial vaginosis, a disease treatable with antibiotics, also increases the risk for premature birth. For the healthiest pregnancy, all types of infections should be avoided.
Environmental Hazards
A fetus can also be at risk because of exposure to natural or man-made chemicals in the everyday environment. For example, a study done on farmers in Wisconsin found that women with higher levels of exposure to pesticides had higher levels of miscarriage and were more likely to have children with leukemia, brain tumors, and other birth defects.
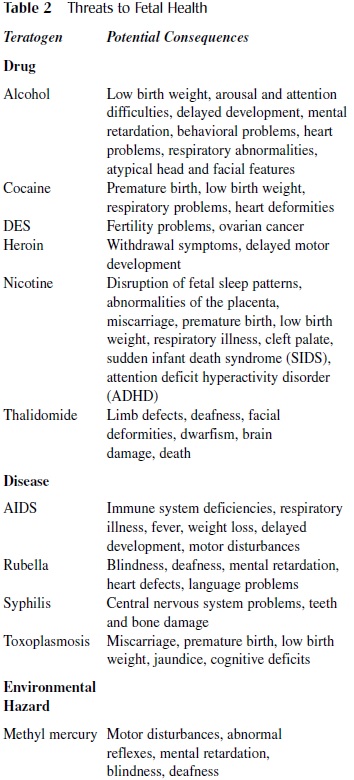 Table 2 Threats to Fetal Health
Table 2 Threats to Fetal Health
Of recent concern is the amount of methyl mercury found in fish. Methyl mercury exists naturally in the environment, and small amounts are not harmful to developing organisms. Levels have risen in recent years because of industrial by-products invading water supplies and being ingested by fish, particularly large fish. Fetuses exposed to methyl mercury through their mother’s diet are at risk for motor disturbances, abnormal reflexes, mental retardation, blindness, and deafness.
Additional Risk Factors
Age
Increased age at pregnancy is associated with increased risk for developmental problems. Beyond the age of 35, a woman is more likely to have a child with Down syndrome, owing to chromosomal abnormalities in her egg supply. The closer a woman moves toward menopause, the more likely hormonal changes will make the uterus less receptive to implantation by a fertilized egg. In addition, older women are more likely to have health problems, which during pregnancy can lead to complications such as high blood pressure, gestational diabetes, and premature birth.
Having a child early in life may also be associated with difficulties. Adolescents are still in the process of growing and increasing bone mass. Pregnancy takes resources from the adolescent’s developing body in order to meet the demands of the growing fetus. One consequence is that adolescent mothers are at increased risk for osteoporosis later in life as a result of sharing calcium during pregnancy. Adolescent mothers are more likely to have infants born prematurely or at low birth weight. Adolescents also have fewer financial resources and are less likely to receive prenatal care than are older mothers.
For most women, the peak of physical health and fertility occurs during their 20s. According to the National Center of Health Statistics, in today’s society, an increasing number of women are waiting until later in life to attempt pregnancy, when the odds of conceiving are lower and the odds of problems are higher. The good news is that this behavioral change has prompted better diagnostic tools and infertility treatments.
Stress
Stress is a normal part of living; however, individual responses to stress may vary considerably. A certain level of stress may seem manageable to one individual and overwhelming to another. The perception of excess stress may cause pregnant women to exercise less, consume harmful substances (e.g., alcohol or nicotine), and eat poorly, all behaviors that can have negative consequences for the fetus.
Stress itself may also create negative consequences for the fetus. During stress, cortisol is released in preparation for a fight-or-flight response. The fetus needs cortisol for maturation of organs, such as its lungs and kidneys; however, chronic stress may lead to greater amounts of cortisol than the developing fetus needs. Dr. Nathanielsz from Cornell University argues that excess cortisol may direct the nervous system to develop a highly sensitive stress response system that overreacts to even mild stressors. Thus, prenatal experiences may design a nervous system that is easily overwhelmed, leading to a chronic stress experience during adulthood.
Prenatal Care
Even in healthy women, pregnancy creates additional challenges for the woman’s body. Early and consistent prenatal care is important to maintain the health of both the mother and the developing fetus. Recent research by David Barker and his colleagues suggests that prenatal experiences may be the most important determinant of overall lifetime health.
Nutrition
The mother is the sole source of nutrition for the developing fetus. Thus, she must meet her own nutritional needs, while simultaneously meeting those of her child. If the woman is not getting enough nutrients, the fetus takes priority. The mother’s body will go without in order to channel more resources to the fetus. The fetus also prioritizes nutrients, with the brain and other essential organs (e.g., heart) receiving the most. As a result, if a fetus lacks adequate nutrients, it may have a head that is proportionally larger than its body.
Pregnant women should increase their caloric intake by 10% to 20%, usually about 400 calories per day. The key to nutritional eating is not eating more, however, but instead choosing the right foods. Some nutrients can have harmful effects in large amounts. For example, vitamin A helps build skin, eyes, and other tissues; however, increased amounts are associated with birth defects in the face, urinary tract, and genitals. Similarly, iron helps create red blood cells, but it also interferes with the body’s ability to absorb calcium and zinc.
Nutritional needs change over the course of pregnancy, in response to the developmental demands of the fetus. For example, during the first trimester, folic acid is necessary for proper development of the neural tube, which will become the brain and spinal cord. During the second trimester, calcium is an important nutrient for bones and teeth to develop properly. Protein is important during the last trimester, when the fetus is actively moving and rapidly growing.
Fetuses that do not receive adequate nutrition are at risk for premature birth, low birth weight, physical defects, nervous system problems, and immune system deficiencies. Nathanielsz argues that the nutritional content of the womb may have even longer-lasting effects by providing information to the developing organism about the scarcity or abundance of resources. In response, the developing nervous system alters its metabolism to either conserve or utilize calories, a program that will continue in the postnatal world. A combination of abundant postnatal food supply and a nervous system designed to conserve calories may explain childhood and adult obesity.
Exercise
Exercise can be beneficial for pregnancy and labor. Good cardiovascular health enables the mother’s circulatory system to meet the increased demands of providing nutrients and oxygen to two people instead of one. Exercise is also linked to mood elevation and decreased stress levels, which may help the expectant mother to avoid other methods of reducing stress, such as smoking or drinking. Researchers have shown that exercise is related to higher birth weights and shorter, less painful labor. Shorter labor decreases the risk for complications that can affect the emerging fetus.
Although exercise is known to be beneficial, certain cautions exist. Exercise should not leave the mother feeling breathless, dehydrated, or overheated. If the mother’s heart rate gets too high, the fetus is at risk for elevated heart rate and oxygen deprivation. A doctor should always be consulted before a pregnant woman begins any fitness routine because certain conditions may require a modified exercise regime.
Multigenerational Effects
Poor prenatal care can affect several generations. For example, a malnourished infant may have developmental limitations, which can then affect that individual’s reproductive ability and fitness later in life. The notion of multigenerational effects is particularly relevant for female fetuses. A female infant will be born with all of the eggs that she will ever have. Thus, that infant’s genetic contribution to her own offspring is formed while she is in her mother’s womb. In this way, an unhealthy womb can affect the current offspring and the generation that is housed in that offspring’s eggs. As argued by David Barker and colleagues, the prenatal care a woman received while still in the womb may be a better predictor of her offspring’s health than will the prenatal care she gets while pregnant.
Summary
The fetal period, which constitutes the longest portion of prenatal development, is a time of physical, behavioral, and cognitive changes. The experiences that a fetus has influence those changes and are influenced by those changes. This process of fetal development creates the framework from which the rest of an individual’s life emerges.
References:
- American College of Obstetrics and Gynecology, http://www.acog.org/
- Bainbridge, (2000). Making babies: The science of pregnancy. Cambridge, MA: Harvard University Press.
- Clapp, F. (2002). Exercising through your pregnancy.Omaha, NE: Addicus Books.
- DeCasper, A. , & Spence, M. J. (1986). Prenatal maternal speech influences newborns’ perceptions of speech sounds. Infant Behavior and Development, 9, 133–150.
- DiPietro, A., Bornstein, M. H., & Costigan, K. A. (2002). What does fetal movement predict about behavior during the first two years of life? Developmental Psychobiology,40, 358–371.
- Nathanielsz, P. (2001). The prenatal prescription. New York: HarperCollins.
- Stoppard, M. (2000). Conception, pregnancy, and birth. New York: Dorling Kindersley.
- Tsiaras, , & Werth, B. (2002). From conception to birth: A life unfolds. New York: Doubleday.
- S. Environmental Protection Agency. (2004). What you need to know about mercury in fish and shellfish. Retrieved from http://www.epa.gov/waterscience/fishadvice/advice.html
- Wingwood, G. , & DiClemente, R. J. (Eds.). (2002). Handbook of women’s sexual and reproductive health. New York: Kluwer Academic/Plenum.