Biopsychosocial Model Background
George Engel’s 1977 article in the prestigious journal Science introduced the biopsychosocial model as a replacement for the traditional biomedical explanatory model in medicine. This article both heralded and instigated a paradigm shift in the fields of medicine and the social sciences, and could be said to have functioned as the primary midwife in the birth of the new interdisciplinary fields of behavioral medicine and psychoneuroimmunology.
The biopsychosocial model seeks to identify the behavioral, emotional, genetic, or pathogenic factors that might alter the body’s internal milieu and thereby facilitate disease processes. The model encourages the clinician to take into account the patient’s attitudes toward illness, life goals, emotional and behavioral reactions, and personality traits and mental disorders, as well as biochemical and structural changes, in understanding the onset and progression of disease. As the model was further articulated, evidence began to amass concerning the role of stress and coping processes in influencing the balance between health and disease. From the other side of the equation, studies demonstrated how an illness alters patients’ social and occupational roles and relationships, which in turn affect the duration and intensity of an illness. There was a growing appreciation for the importance of the bidirectional communication between patients and their health care providers as well as the wider psychosocial environment in influencing patients’ response to medical care and recovery from illness.
Historical Pathways
In both research and clinical practice, the biomedical model since the time of Pasteur had focused on discovering discrete, molecular causes of disease. Research conducted according to this largely unchallenged model was often spectacularly successful in uncovering the etiology of acute infectious diseases and developing cures. As these diseases were gradually conquered or controlled and as more chronic disorders such as cancer and heart disease emerged as the predominant causes of death in the second half of the 20th century, both clinicians and researchers began to appreciate the importance of the interaction of multiple factors in the onset, progression of, and recovery from chronic disorders.
Stress
Arguably, the most important of these factors was stress, a phenomenon first named by Hans Selye at McGill University. Richard Lazarus, a major theoretician and researcher in this area, defined stressful situations as those novel, unpredictable, and/or uncontrollable situations in which individuals are faced with environmental or other demands that exceed their ability to cope. In the mid-1970s the physician Ray Rosenman and his colleagues reported that the response to stress that they called the Type A behavior pattern was a significant risk factor for coronary heart disease.
Research on the pathogenic components of Type A behavior, particularly hostility, was invigorated and solidified by methodology from the rapidly growing discipline of health psychology, formally recognized in the United States in the late 1970s (and a decade later in Europe), even though psychologists had worked for decades in the areas of health and illness. In the early to mid-1980s, the British psychiatrist Steven Greer and the American psychologist Lydia Temoshok led teams investigating the role of emotion management (expression or repression) and coping styles (e.g., the Type C coping style) in the progression of cancer. In the 1990s, The Belgian psychologist Johan Denollet investigated the relationship of Type D personality (high negative affectivity and high social inhibition) to coronary heart disease.
Psychosomatic Medicine
Psychosomatic medicine, a field that grew out of the psychoanalytic approach to medicine, was a parallel and contributory influence on the evolution of the biopsychosocial model. By the 1950s, psychosomaticists had a list of seven ailments thought to have a psychological as well as a physical component to their etiology: peptic ulcers, ulcerative colitis, hypertension, hyperthyroidism, rheumatoid arthritis, neurodermatitis, and asthma. Perhaps the most influential research in this field in terms of foreshadowing the development of the biopsychosocial model was conducted by psychiatrist George F. Solomon and the psychologist Rudolph Moos. Their now-classic 1965 study published in Psychosomatic Medicine demonstrated that a psychological variable—integrated and “super healthy” psychological functioning—can prevent the process by which a predisposing biological agent—the rheumatoid factor (an antibody found in the blood of patients with rheumatoid arthritis and considered a genetic marker)—would otherwise lead to overt illness—rheumatoid arthritis, a severe autoimmune disease that affects the connective tissue of the joints.
Immune System Connections
A 1964 theoretical paper by Solomon and Moos on emotions, immunity, and disease was clearly on the threshold of a new paradigm. By 1966, Solomon was using “psychoimmunology” to label his laboratory research with the immunologist Alfred Amkraut, including their remarkable study published in 1972, which showed the importance of individual differences in modulating the effects of stress on tumors in mice. Influenced by pioneering but largely unknown research by Russian scientists, including Elena Korneva on the role of the hypothalamus in immunity, Herbert N. Spector championed the term “neuroimmunomodulation.” But it was experimental psychologist Robert Ader, who had worked with the immunologist Nicholas Cohen on the classic experiments showing that rats’ immune responses could be behaviorally conditioned, who ended up with the winning term for the field, psychoneuroimmunology.
Mind-body Medicine
Research into this uncharted territory received a shot in the arm, so to speak, from the popular press. First published as an article in the New England Journal of Medicine in 1976, Norman Cousins’ Anatomy of an Illness, was an anecdotal account of his personal triumph over severe illness, the healing power of laughter, and the importance of the patient—physician relationship. The book, as well as the cancer surgeon Bernie S. Siegel’s 1986 book, Love, Medicine, and Miracles, stimulated thousands of articles and books dealing with aspects of mind-body medicine, sometimes referred to as “alternative” or “complementary” medicine. A marker of how far the field has come was the establishment of a National Center for Complementary and Alternative Medicine as part of the National Institutes of Health. Some critics, however, have argued against the “medicalization” of the field of mind-body medicine, in that clinicians in both standard and alternative medicine rely on randomized controlled clinical trials as the only method to document the effectiveness of an intervention, and NIH funding follows. To the extent that such trials seek to control and eliminate multiple factors and interactions, they are antithetical to testing the “real world” application of the biopsychosocial model.
Systems Theory
Homeostasis, the ability or tendency of an organism to maintain internal equilibrium and a state of health by regulating its physiological processes, was first described in 1935 by Walter Cannon. This major tenet of systems theory is central to an understanding of health and disease. In 1983, Temoshok adapted elements from stress theories and the systems theories of Tart, Battista, and John concerning consciousness and hierarchically organized mental subsystems to propose a multidimensional theory of emotion, adaptation, and disease. According to this model, the dynamic equilibrium of homeostasis is disrupted when there is too much or too complex information, internal or external, which cannot be integrated into consciousness, causing distress. The process of repression, by which the cognitive content and the affective meaning of the information are split and one or the other relegated to subsystems below the level of consciousness, reduces distress and allows a precarious balance to be re-established. However, there is a price to pay for this state of uneasy equanimity. To the extent that information salient to mental or physical health is inaccessible to consciousness, this information or cue cannot be acted on nor can the stressful situation be resolved. Temoshok theorized that extreme levels of stress, stress early in life, and/or very inadequate coping resources lead to information accommodation via the process of repression at increasingly more primitive mental subsystems, resulting in maladaptive mental and physical functioning, and, eventually, increasingly severe mental and physical disorders.
Psychologist Gary Schwartz (1990) argued that some attention to levels of distress is needed for feedback mechanisms and homeostasis to function so that the organism maintains health. A repressive style in which the meaning of emotions or bodily sensations is cut off from conscious awareness disturbs these feedback mechanisms such that the normal homeostatic process in which arousal is followed by return to baseline goes awry. Temoshok interpreted her findings on the relationship of the Type C coping style to cancer progression along parallel lines, in that the Type C style has a large repressive component in addition to nonrecognition and nonexpression of emotion. Maladaptive coping patterns such as Type C represent deviations from the inverted U-shaped function that characterizes homeostasis (commensurate arousal in response to stimuli followed by return to baseline) in that they fail to recognize, respond appropriately to, and/or resolve stressors. This coping pattern tends to keep the physiological stress response— and Cortisol immunosuppressive effects—chronically engaged, with implications for vulnerability to immunologically mediated diseases.
These theories implicate as mediating mechanisms the existence of bidirectional pathways between neuroendocrine and immune processes, as established by numerous psychoneuroimmunologic studies. More recent research has demonstrated that, in addition to neurotransmitters and hormones, brain function is modulated by neuropeptides. Receptors for neuropeptides are found throughout the brain, particularly in the limbic system areas that mediate emotion, as well as on various cells in the immune system. Candace B. Pert, now at Georgetown University Medical Center in Washington, D.C., who conducted pioneering research on opiate receptors in the brain, was the first scientist to promulgate the conceptual shift that neuropeptides (or as they are now called more generally, “cytokines” and “chemokines”) and their receptors are the communicating link among the mind, the brain, and the endocrine and immune systems (Pert et al., 1985). In 1996, chemokine receptors were discovered to play a key role in HIV’s ability to enter cells. The results of studies showing that specific chemokines have been shown to block viral receptors, and thus HIV entry into cells, has opened up new possibilities for biomedical treatments targeted at blocking viral receptors. To the extent that certain psychosocial factors may stimulate chemokine production that inhibits HIV, it is logical that research into how these factors may be engaged may constitute the basis for a “natural” biopsychosocial anti-HIV intervention.
Elaborating the Biopsychosocial Model
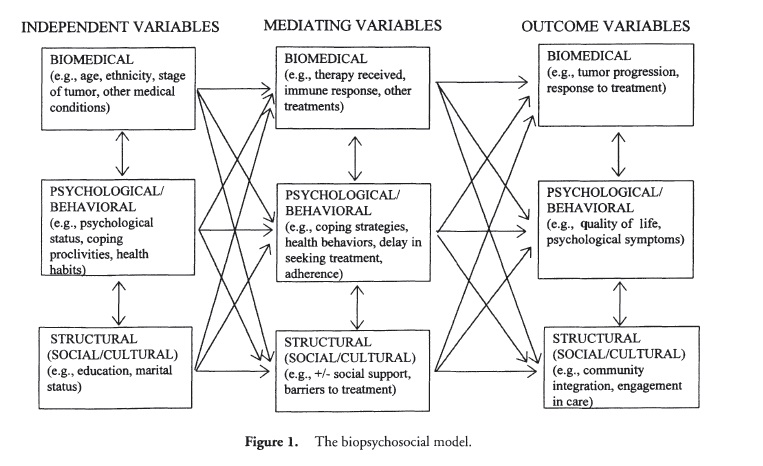
A major challenge for researchers in health psychology and behavioral medicine is to understand how stress or other psychosocial factors may mediate the development or exacerbation of an illness. Evidence suggests that there is not just a single route involved (see Figure 1), in that stress may result in negative health outcomes by direct effects on organ systems (e.g., increases in blood pressure, muscle tension, Cortisol, gastric motility), by indirect biological effects (e.g., exacerbating or triggering a disease process in an already genetically vulnerable individual), or by increasing risk behaviors (e.g., smoking, alcohol consumption) that contribute to disease processes.
Much research in health psychology has focused on individual beliefs, attitudes, cognitions, and behaviors as well as environmental factors (e.g., social support, the treatment environment, doctor-patient communication) that affect medically salient processes and outcomes (e.g., adherence to medical treatment, risky behaviors). Another vigorous area of research focuses on the psychological concerns and coping of patients with chronic diseases, disabilities, and stressful medical procedures. On the same coin of the realm as behavioral medicine but on the flip side is the field of behavioral health, which encompasses health promotion, education, and prevention (e.g., accident prevention, immunization, nutrition, physical fitness and exercise, occupational safety and health, and changing health-damaging lifestyles.)
Let us consider the phenomenon of HIV/AIDS in the context of the biopsychosocial model and Figure 1, beginning with the premise that HIV not only affects the biomedical sphere of the person with the infection, but also significantly affects the psychological and social realities of any person touched by HIV. A further tenet of the biopsychosocial model is that the health and the sense of well-being of individuals affected by HIV are not dependent solely on the achievements of biomedicine. To the extent that psychosocial and behavioral variables influence susceptibility to HIV infection, quality of life, and possibly progression of HIV disease and longevity, then these variables become critical to consider in HIV prevention and intervention. A problem of this magnitude requires a comprehensive approach to inform medical, psychological, and public health intervention and prevention efforts.
The biopsychosocial model is the logical theoretical underpinning of this comprehensive approach. Elaborating the boxes in Figure 1, understanding the direction and strength of the arrows, as well as which boxes and arrows are highlighted for specific diseases and disorders constitute a worthy challenge for biopsychosocial researchers in the 21st century.
References:
- Ader, R. (Ed.). (1981). Psychoneuroimmunobgy. San Diego, CA: Academic. Cousins, N. (1979). Anatomy of an Illness. New York: Norton. Engel, G. L. (1977). The need for a new medical model: A challenge for biomedicine. Science, 196, 129-136.
- Pert, C B., Ruff, M. R., Weber, R. J., & Herkenham, M. (1985). Neuropeptides and their receptors: A psychosomatic network. Journal of Immunology, 135, 820-826.
- Schwartz, G. E. (1990). Psychobiology of repression and health: A systems approach. In J. L. Singer (Ed.), Repression and dissociation (pp. 337-386). Chicago: University of Chicago Press.
- Solomon, G. E, Kemeny M. E., and Temoshok, L. (1991). Psychoneuroimmunologic aspects of human immunodeficiency virus infection. In R. Ader, D. L. Felten, & N. Cohen (Eds.), Psychoneuroimmunology (2nd ed., pp. 1081-1111). San Diego, CA: Academic.
- Solomon, G. E, and Moos, R. H. (1964). Emotions, immunity, and disease: A speculative theoretical integration. Archives of General Psychiatry, 11, 657-674.
- Temoshok, L. (1983). Emotion, adaptation, and disease: A multidimensional theory. In L. Temoshok, C. Van Dyke, and L. S. Zegans (Eds.), Emotions in health and illness: Theoretical and research foundations, (pp. 207-233). New York: Grune & Stratton.
- Temoshok, L. (1990). On attempting to articulate the biopsychosocial model: Psychological-psychophysiological homeostasis. In H. Friedman (Ed.), Personality and disease (pp. 203-225). New York: Wiley.
- Temoshok, L. (2000). Complex coping patterns and their role in adaptation and neuroimmunomodulation: Theory, methodology, and research. Annals of the New York Academy of Science, 917, 446-455.
Back to Health Psychology.